Mind, Body, Mouth, it’s all connected. Dental Health Week 2023 – Pregnancy

There is early evidence supporting the association between periodontitis and adverse pregnancy outcomes including preterm birth, low birth weight and preeclampsia.
There are several factors proposed to explain the association including:
- Inflammatory mediators
- Oral bacterial dissemination
The microbial imbalance in the mother’s oral cavity is thought to be linked to maternal immunity and infant health leading to some studies hypothesising this imbalance to be the link between the mouth and the adverse pregnancy outcomes.
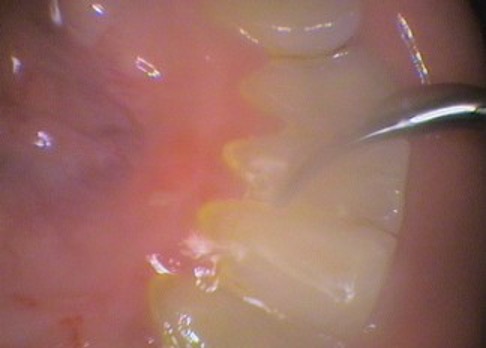
Pregnancy related pathology in the oral cavity is most commonly found in gingival (gum) tissue. Gingival inflammation is plaque induced but modified by oestrogen and progesterone during pregnancy.
Studies have identified that these hormones can alter the micro-organism under the gums, compromise periodontal ligament cells (which hold the tooth to the bone) and change the maternal immune response. Gingivitis (gum inflammation) typically precedes periodontitis (inflammation of the ligament that holds the tooth to the bone).

During pregnancy, there is overproduction of oestrogen and progesterone with the values shifting depending on the stage of reproduction. Some studies have suggested that these hormones can affect the species of bacteria present in the periodontium causing an increase in pathogenic A. actinomycetemcomitans, S. mutans and P. gingivalis in pregnant women. Studies have also noted an increase of periodontal pathogens in women that had adverse pregnancy outcomes. Another study demonstrated that hormones could act as an essential growth factor for some of the pathogens.
The hormones are also attributed to affecting periodontal ligament cells by either changing the effectiveness of the epithelium as a barrier to bacterial insult or by affecting the capacity of collagen repair. Oestrogen and progesterone have also been shown to increase the rate of folate metabolism in gingival tissue thereby, leaving insufficient quantities for tissue repair.
Hormones have also been involved in the immune response to oral pathogens with the neutrophil (type of white blood cell) function being impaired. This may increase the susceptibility of pregnant women to gingival inflammation.
The mechanisms by which periodontal disease is linked to adverse pregnancy outcomes has been categorised into direct and indirect pathways.
The direct pathway involves passage of oral microorganisms to the placenta through the blood or through the genitourinary tract. The presence of these bacteria may lead to development of infection and may to an increase the risk of preterm birth.
Indirectly, the association is thought to occur due to an increase in inflammatory mediators in the circulation and lead to early contractions.
Further research is required but there is sufficient evidence to indicate that monitoring and management of oral health diseases in pregnant patients is vital in reducing the adverse outcomes from occurring.
We can’t control the hormones but we can control the oral inflammation and the oral microorganisms. Dental treatment during pregnancy is safe. People planning to become pregnant should have dental treatment done ideally beforehand to minimise the impact that hormonal fluctuations have on oral health.
Need an Appointment?
If you’d like to book an appointment with the dentist at Seymour Dental then call us in Dulwich Hill, Sydney on (02) 9564 2397 or
contact us
Next week
Halloween 2023